Quality of air can boost your immune systems against COVID-19
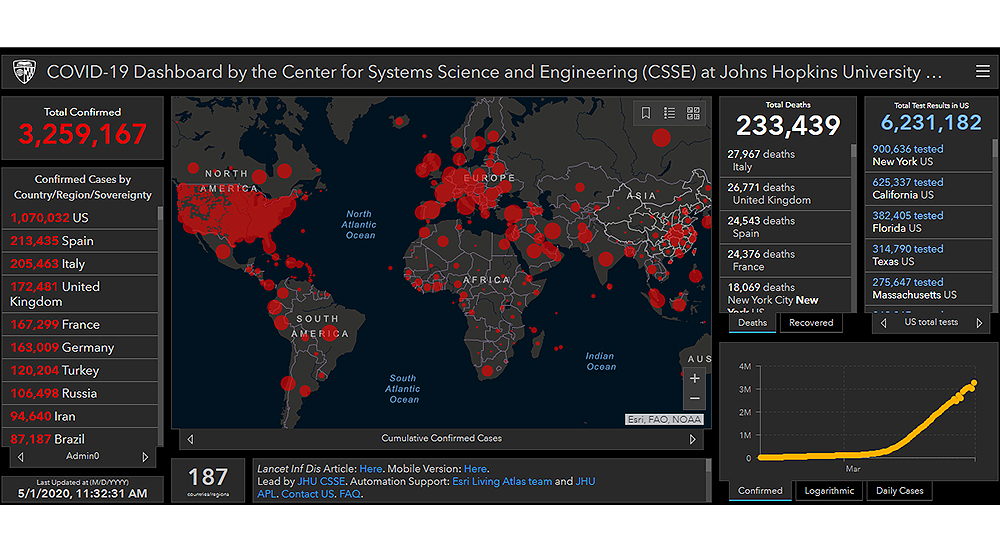
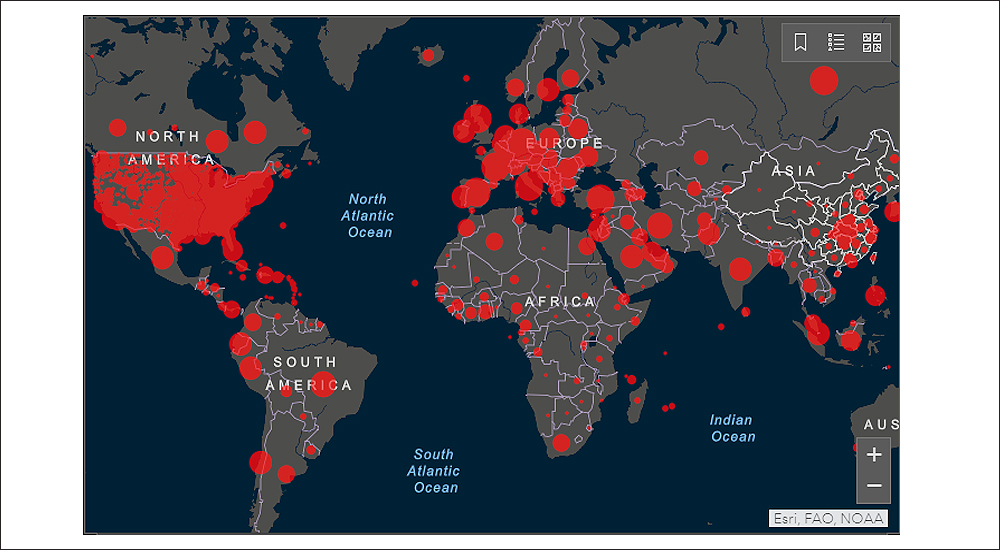
The number of globally infected persons from COVID-19 are sharp racing towards the 5 million mark. Amongst the medical community and experts at large, the propagation mechanisms of COVID-19, appears to have reached some sort of consensus. Continuous social mixing of humans and continuous aggregation of humans, whether indoors or outdoors, appears to be a recipe for fast propagation. This has been repeatedly demonstrated in cruise ships, during religious congregations, staycations whether in the outdoors or hotels, and other closed systems such as the lavatory and bathrooms.
Separation of humans, short contactless engagements, and fresh circulation of air, appear to help reduce the propagation. In addition we have the standard medical adherence and practices towards highly infectious diseases that include full body suits, or in its absence – gloves and masks, and continuous sanitised conditions.
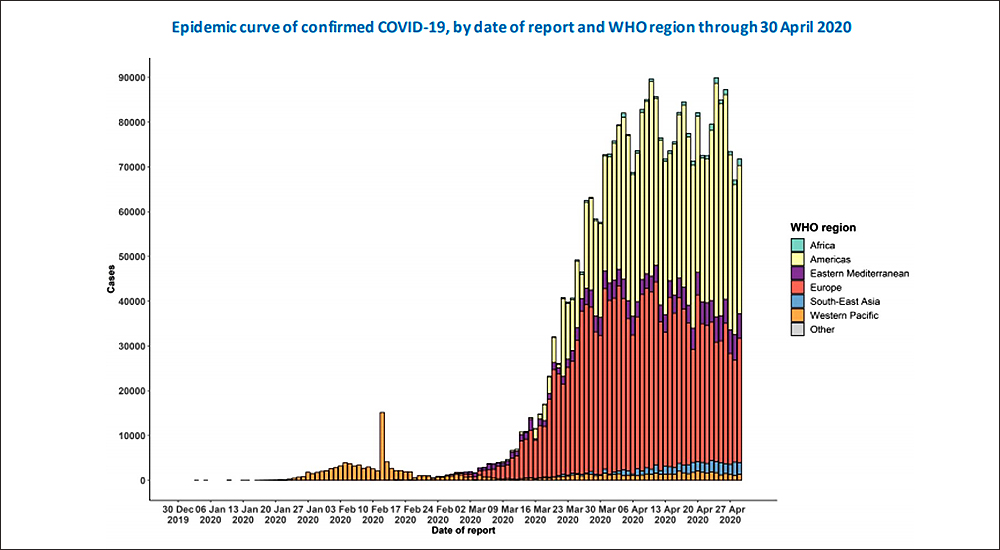
Many global models have pointed out the rapid propagation of COVID-19, across the cold temperate zones of the world. Inversely, these models show a lower propagation across the warmer belts of the world, in comparison to a higher propagation across the colder belts. However, there is as yet no empirical and definitive research about the correlation of global temperature zones and the spread of COVID-19.
Lack of testing centres, lack of reach in rural areas, lack of recorded deaths, continue to negatively reduce and skew the real picture of the pandemic across Third World countries, perhaps much, much more than what variance the models would provide. In short, under reporting in a large number of countries, may be preventing a true understanding of the transmission mechanism of COVID-19, in other climatic belts.
COVID-19: A modern day pandemic
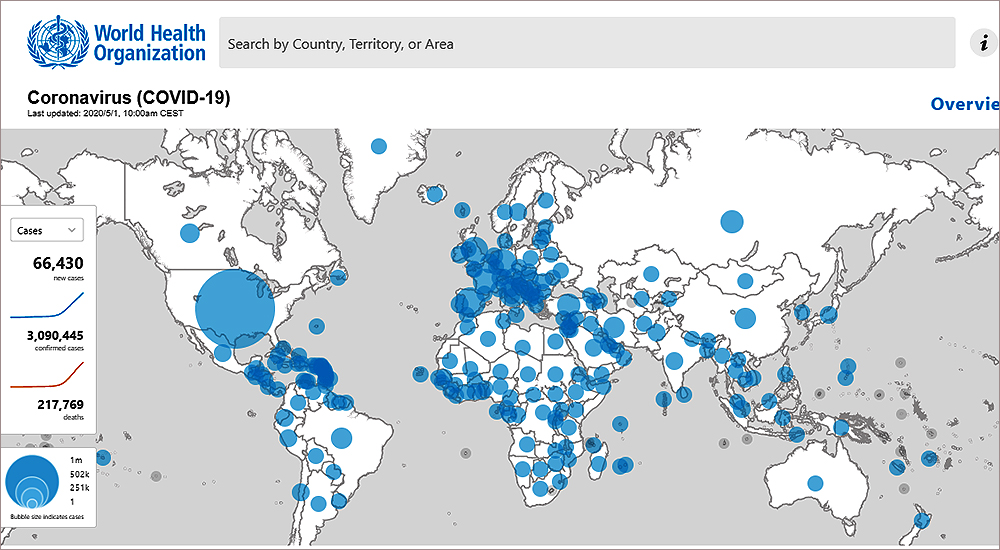
Moving forward, The World Health Organisation has recognised the link between poor air quality and severity of propagation of COVID-19. Dr Maria Neira, Director, Public Health, Environment and Social Determinants of Health Department at the WHO, pointed out that countries with high pollution levels, like those in Latin America, Africa and Asia, need to ramp up their CODID-19 operations. People in these countries suffer from pollution-related conditions and can develop a severe form of COVID-19.
Available evidence indicates that COVID-19 virus is transmitted during close contact through respiratory droplets such as coughing and by fomites. The virus can spread directly from person to person when a COVID-19 case coughs or exhales producing droplets that reach the nose, mouth or eyes of another person. Alternatively, as the droplets are too heavy to be airborne, they land on objects and surfaces surrounding the person. Other people become infected with COVID-19 by touching these contaminated objects or surfaces, then touching their eyes, nose or mouth. According to the currently available evidence, transmission through smaller droplet nuclei airborne transmission that propagate through air at distances longer than 1 meter is limited to aerosol generating procedures during clinical care of COVID-19 patients.
As such, WHO continues to recommend that everyone performs hand hygiene frequently, follows respiratory etiquette recommendations and regularly clean and disinfect surfaces. WHO also continues to recommend the importance of maintaining physical distances and avoiding people with fever or respiratory symptoms. These preventive measures will limit viral transmission. Since the start of the COVID-19 outbreak, and in alignment with available evidence, WHO maintains the recommendation, in the context of droplet and contact precautions for the use of medical masks for regular care of COVID-19 patients and respirators N95, FFP2 or FFP3 for circumstances and settings where aerosol generating procedures are performed.
Excerpted from WHO Coronavirus disease 2019, COVID-19, Situation Report 66, dated 26 March 2020.
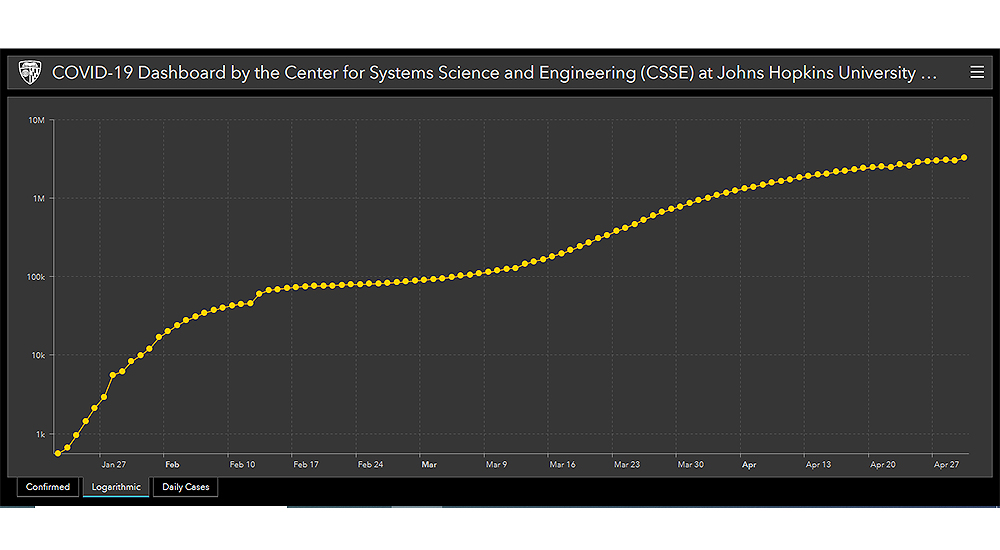
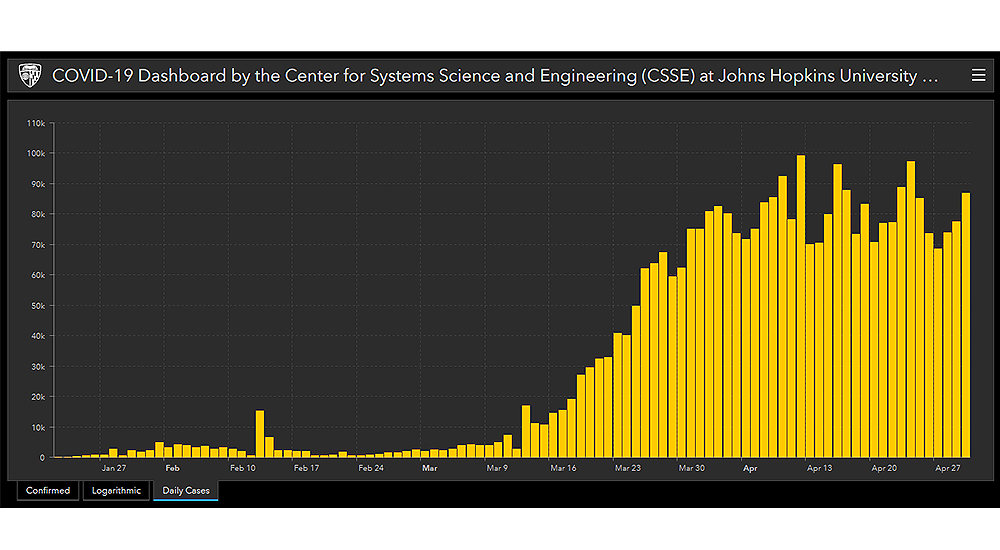
Is the COVID-19 global infection curve flattening?
Managing indoor atmospherics
So while, outdoor air is beyond the control of citizens at large, there is a school of research and thought that advocates the management of indoor air conditions, inhibiting the propagation of COVID-19, indoors. Indoor air conditions are determined by the intrinsic purity of air, temperature and relative humidity. Linked to indoor air conditions, is also the condition of indoor surfaces.
The founder of Amfah India, Research Analyst and Indoor Air Quality expert, Mansoor Ali says, “The correct indoor environment mix, will strengthen people’s immune systems and keep them safe from the current outbreak. This combination is a blend of optimum air quality, temperature and humidity.”

Ali has prepared his findings from the results of his studies into COVID-19 from Europe and US. Lives have changed in the wake of the pandemic, including the way we communicate, eat and stay safe from virus strains. These safety measures include avoiding conditions which would lead to sneezing, coughing and sore throats and holds for summers around the corner.
Sanitised, ventilated spaces also add to safe living conditions for everyone, whether at homes or outside. The positive air quality that is currently developing around us, is an unintentional outcome of the lockdown.
Why is the COVID-19 infection curve so different in the geographies?
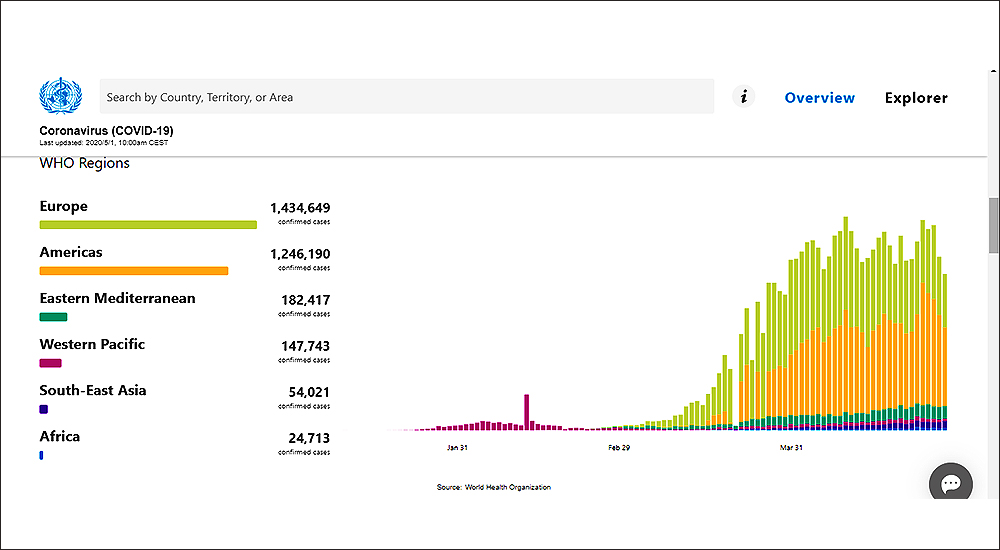
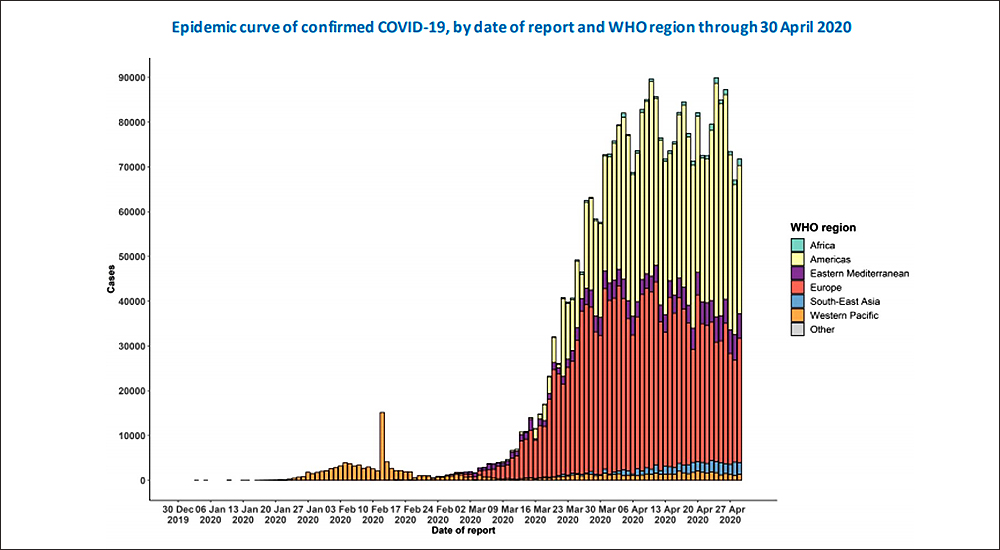
Source: Coronavirus disease 2019 Situation Report – 101, dated 30 April.
Managing the human body
Protecting the human mouth and nose as entry point for COVID-19 is an integral part of Ali’s, cold and wet atmospheric theory. Avoiding cold beverages and foods is an important measure against COVID-19. Frozen foods, cold beverages and poor air humidity can act as irritants, which will make people sensitive and exhibit flu-like symptoms and further get infected with COVID-19 from human transmission or through infected surfaces. Human protection also includes managing lifestyle and behaviour patterns according to the Indian division of Publicis Groupe’s.
“COVID-19 is spreading due to human transmission and surface-based contamination. While social distancing and cleansing measures help, we need to boost our immunity levels as well,” explains Ali. Research at Amfah India proposes doing this with an indoor air quality of 2.5 PM, 24-degree room temperature and optimum humidity levels. Research has confirmed, maintaining a relative humidity of 40-60% will prevent transmission and deactivation of surface-based contamination.
There is on-going research into the incidence of cold and cough as a sign of the upcoming crises. There is enough research now linking better air quality to lesser casualties, since COVID-19 impacts our breathing abilities. Says Ali, “Focus on immunity and avoid anything which can attract cold and cough.”
Workers and workplace
Employers need to put practices in place to guide employees through safety measures. Create a basic hygiene and social distance strategy, communicate it across the workplace and ensure that everyone adheres to it. Employers should also check and maintain indoor air quality, especially if this air is being re-circulated through a building. With poor air quality, even a single infected person can spread the disease to the rest of the staff. Ali recommends the use of humidifiers, to maintain 50% relative humidity, which can contribute to an efficient immune response.
It takes at least 45 days to prepare and implement safety measures and guidelines inside a large scale infrastructure. Cleaning and disinfecting surfaces, social distancing, safeguarding from the entry of positive patients and carriers, are now relatively well known practices. Institutions should explore ways to build a sanitised ventilation system, reducing the chances of pathogens in the air. Employees and staff need to have classroom and hands-on training on hygiene levels and handling possible contingencies.
As research agencies aggregate patient data and build large scale propagation models, both qualitative and quantitative recommendations are likely to emerge. Over time these will finally improve leading to a real life scenario model.
Key takeaways
- It takes at least 45 days to prepare and implement safety measures and guidelines inside a large scale infrastructure.
- There is on-going research into the incidence of cold and cough as a sign of the upcoming crises.
- Use of humidifiers, to maintain 50% relative humidity are recommended, which can contribute to an efficient immune response.
- Under reporting in a large number of countries, may be preventing a true understanding of the transmission mechanism of COVID-19.





